
Thursday: Fitness Don’s (Hip Flexor Stretching)
Maybe You Shouldn’t Stretch Your Hip Flexors?
Hip flexor and hamstring stretches are the most popular stretches amongst runners and fitness enthusiasts.
However, it is rarely discussed whether or not such stretching is appropriate.
I have previously discussed how core stability (positional breathing drills) exercises can alleviate hamstring tightness without stretching: https://www.flexibilityrx.com/can-you-breathe-away-hamstring-tightness/.
I have also discussed the need to understand why shoulder internal may be limited before stretching the shoulder in this post: https://www.flexibilityrx.com/reconsidering-the-sleeper-stretch/.
Now let’s look at another potentially disadvantageous exercise – hip flexor stretching.
Here are three considerations to factor in before stretching your hip flexors.
#1: Do I Have Laxity in My Anterior Hip Ligaments?
The Postural Restoration Institute is unique in their treatment approach to musculoskeletal disorders not only in their discussion of asymmetry and respiration, but in their assessment of pathological stabilization patterns.
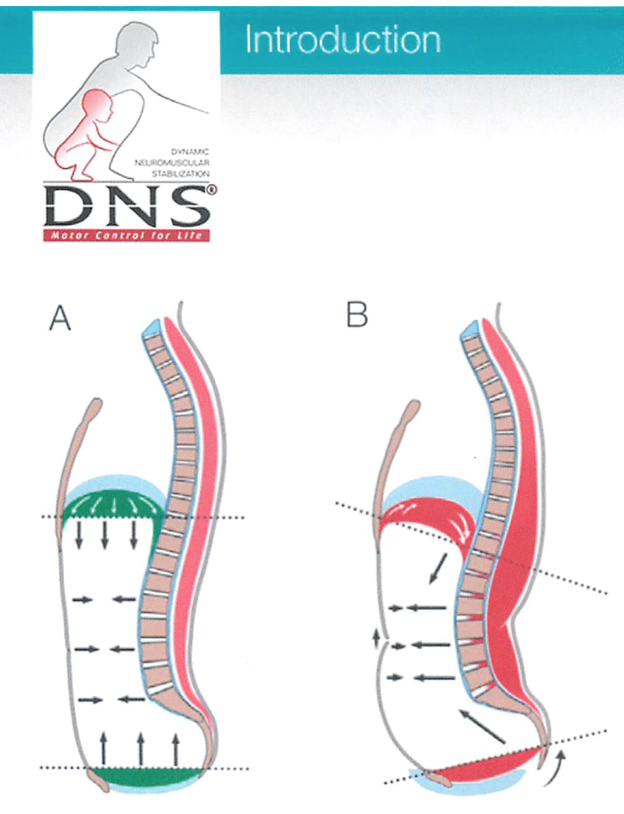
In my previous post (Reclaiming the Sagittal Plane) I discussed the Extension Compression Stabilizing Strategy (ECSS) that the Prague School of Rehabilitation (DNS) has put forward. Basically, when muscle balance that provides core stability is lost, different muscles have to compensate for movement and upright posture. This compensation pattern involves hyperactive spinal erectors, overlengthened hamstrings, and a concentric abdominal wall that maintains a position of an elevated ribcage, hyper lumbar lordosis, and an oblique positioning of the diaphragm and pelvic floor.
The Postural Restoration Institute refers to this dysfunction as a loss of a Zone of Apposition. The muscles that hold this tensional balance in place cannot properly oppose the diaphragm so that it can obtain a domed position during exhalation and maintain spinal stabilization during an inhalation.
PRI emphasizes the need for hamstring and abdominal integration to support the diaphragm. When this ZOA is lost posture and movement will be compromised in an ongoing compensatory strategy (what DNS refers to as the ECSS).
PRI has contributed to the understanding of this pattern by providing assessments to determine if an individual has ligament laxity.
Using Tom Myers concept of primary and secondary curves – when someone uses an Extension Compression Stabilizing Strategy secondary curves like the lumbar spine and knees begin to act as primary curves. In other words, curves like the lumbar spine that are held in place by myofascial (not by bony support) are exaggerated (lumbar hyper lordosis) or eliminated (knee hyperextension).
This involves both tight (shortened) musculature and overlengthened musculature. This pattern causes someone to over-rely on their joints for stability (locking out their knees) or compressing their lumbar spine. It is in this situation that ligaments become overstretched.
Tom Myers has helped us reframe how we think of ligaments:
http://www.fascialfitnesstoday.com/Images/massage0311.pdf.
In summary, ligaments are tensioned and act through muscular and connective tissue force transmission. This is good news because this means that we can re-tension ligaments by retraining the muscles and fascia that support them.
The Postural Restoration Institute teaches us how to do that in their courses. This article will focus on understanding how to assess the ligaments of their anterior hip so that we can ensure that stretching of the anterior hip (hip flexor stretches) is appropriate.
—
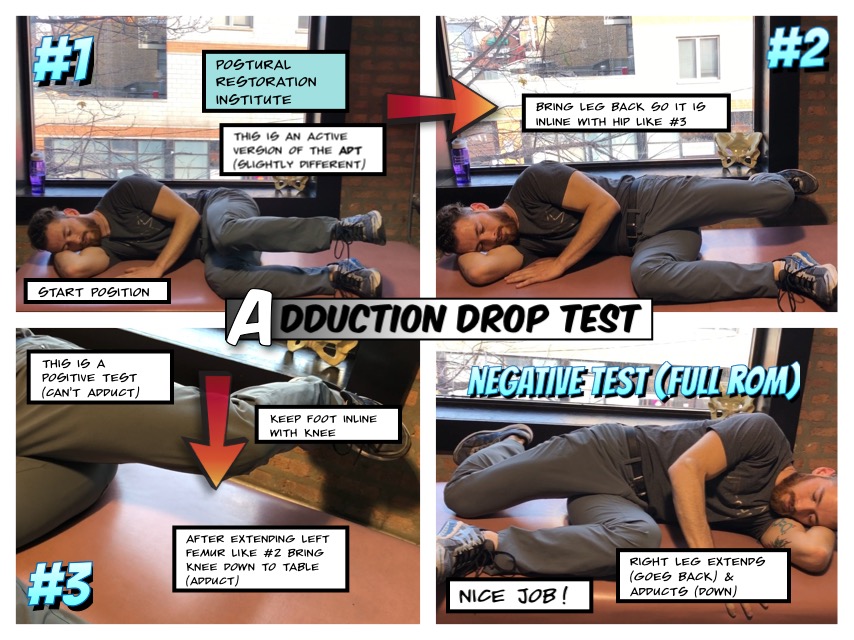
To assess the anterior ligaments of your hip and rule out pathology you will need to perform two tests. PRI utilizes these two tests passively (the client’s limbs are moved passively). The first test is not quite the same when done active as it involves frontal plane control of the hip joint. Just keep that in mind when performing this test.
However, many individuals who are extremely tight in their hip will be strongly limited in the first test regardless. I say this because the second test is only of use if the first test is limited (positive). In other words, the second test SHOULD be positive (limited) if the first test is positive.
If the Adduction Drop Test is Positive then we WANT protective tension (tightness) with the second test (Thomas Test).
Scenario #1: + Adduction Drop Test & + Thomas Test = Intact Hip Ligaments
Scenario #2: + Adduction Drop Test & – Thomas Test = Anterior Hip Laxity
a third scenario is possible…
Scenario #3: – Adduction Drop Test prevents us from using the second test
So, you are either tight (in a good way) and can stretch (Scenario #1) or you have ligament laxity (Scenario #2) and should completely avoid hip flexor stretching altogether.
In Scenario 2 note how you will see be limited in the Adduction Drop Test – basically your ability to adduct your hip and achieve hip extension is STILL LIMITED despite your laxity.
Scenario #3: Unless you have severe pathology (outside the scope of this article) your hip is in a neutral position – you can extend and adduct your hip and hip flexor stretching is probably not worth your time anyway.
—
Read the above section a few times before performing the tests. I know it is confusing at first, but it is certainly worth your time to go through this assessment process.
The following two tests are taught by PRI in their Myokinematic Restoration Course:
https://www.posturalrestoration.com/programs-courses/introductory-courses/myokinematic-restoration
While both of these tests can be considered standard orthopedic tests used by physical therapists (The Obers Test and the Thomas Test) how PRI interprets and uses these test is completely different than a how a normal physical therapist would use them. This enables us to draw different conclusions especially in regard to ligament laxity.
Test A: Adduction Drop Test (variation of)
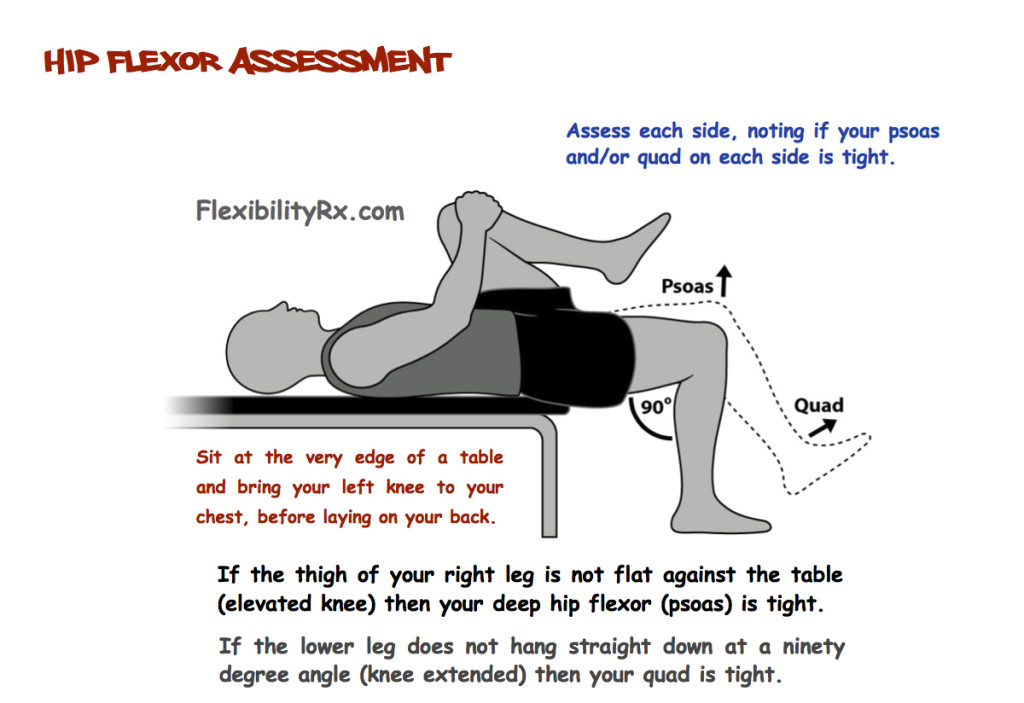
Test B: Thomas Test (Extension Drop Test)
You can forget about knee flexion/extension with this test (influence of the quads). What you are looking for is whether or not the free hanging knee touches the table or not. Tightness (a positive test) would be indicated by the right knee above not lying inline with the hip. The knee would be elevated above the line of the torso. The graphic above depicts a negative test, the dotted line indicates a positive test (raised knee).
#2: Soft Tissue Restrictions are Driven by Neurology
Pavel Kolar has a great saying, “Trigger points are in the brain.”
What this means is that when posture and movement is compromised our brain has to provide a secondary strategy of stabilization. It does this by over tensioning certain muscle groups which results in the formation of trigger points.
Self-myofascial release and stretching certainly have their place (I am a Fascial Stretch Therapist) but we need to understand that there is a need to re-education the nervous system through good movement.
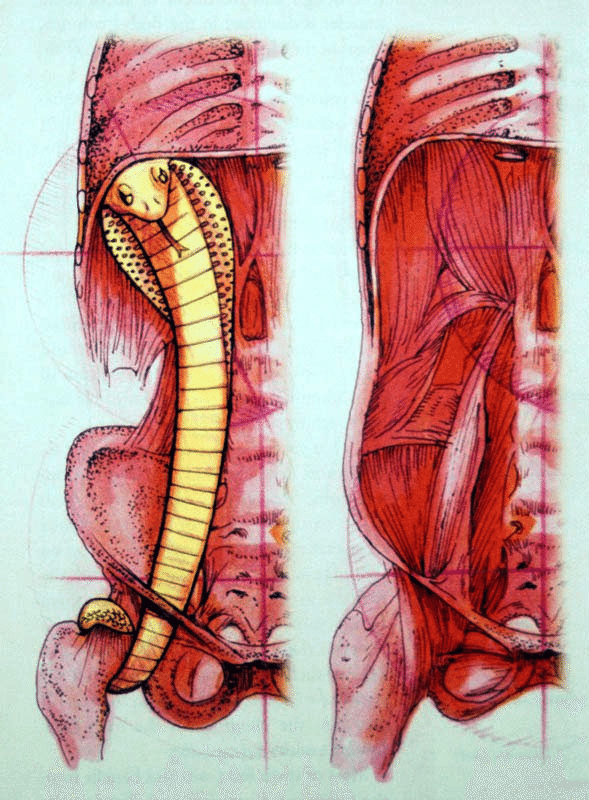
This movement needs to incorporate proper respiration. The psoas muscle group connects not only to the spine but to the diaphragm. If we don’t retrain breathing patterns we will never reduce hypertonicity of the hip flexors.
To influence breathing patterns and core stabilization we need to train the hamstrings and abdominals (internal obliques and transverse abdominis).
After doing this we can re-assess hip flexor tonus and then see if stretching is appropriate (assuming someone has intact anterior hip ligaments).
#3: Am I Able to Maintain a Stabilized Position of the Core While Stretching?
This third consideration has already been touched on multiple times and any good coach or trainer knows how to take someone through a good hip flexor stretch.
Here are some considerations though:
Excessive anterior pelvic tilt should be eliminated
There should be no excessive lumbar lordosis
Fully exhale to set the ribcage down into a neutral position
Caution should be exercised taking the hip past 90 degrees
A reach with the same side arm helps targets the fascia
Lateral movement of the hip (side to side) frees up related fascia
Rotation movement of the torso helps target fascia
Breathe inhaling/exhaling with the movement
Overstretching the anterior hip even without the presence of ligament laxity often involves poor neurological priming of movement patterns. The overarched low back in a lunge stretch will manifest in an overarching back during functional movement patterns.
Some closing thoughts…
Manual Therapy/Stretching Versus Self Stretching
As a Fascial Stretch Therapist who does take the hip past neutral during assisted stretching – I first rule out ligament laxity. I then perform hands on manual therapy to the psoas before stretching. Freeing the fascia between the iliacus and psoas (a technique more suited to hands on work) also opens up this range of motion. I then use PNF (neurological principles) during stretching as taught by the Stretch to Win Institute.
Stretching in a Group Setting
One of the reasons I am weary about hip flexor stretching is how it is often performed during a warmup in a group setting. Some stretches are more appropriate than others when used without proper assessment in a group setting. Lat, calf, and pec stretches for example tend to be on the safer side whereas hamstring, hip-flexor, and low back stretches require more caution and in-depth assessment.
First Consider Why the Psoas is Chronically Tight
Tightness after a run is different than chronic hip flexor or hamstring tightness. Post workout stretching that takes the body back through a full range of motion is definitely more appropriate than pre-workout stretching that has already failed to resolve chronic tightness or structural misalignment. Since the psoas and diaphragm are so interconnected always first consider a positional breathing drill on your own before stretching.
Please share this article with a fellow coach or gym member.
– Kevin J Kula, “The Flexibility Coach”


Leave A Reply (No comments so far)
You must be logged in to post a comment.
No comments yet